The liver is one of the most essential organs in the body, playing a crucial role in detoxifying, aiding digestion, storing nutrients, and fighting infections. However, like any vital organ, the liver is vulnerable to various diseases and conditions. Among these, fatty liver disease is becoming increasingly common in today’s world.
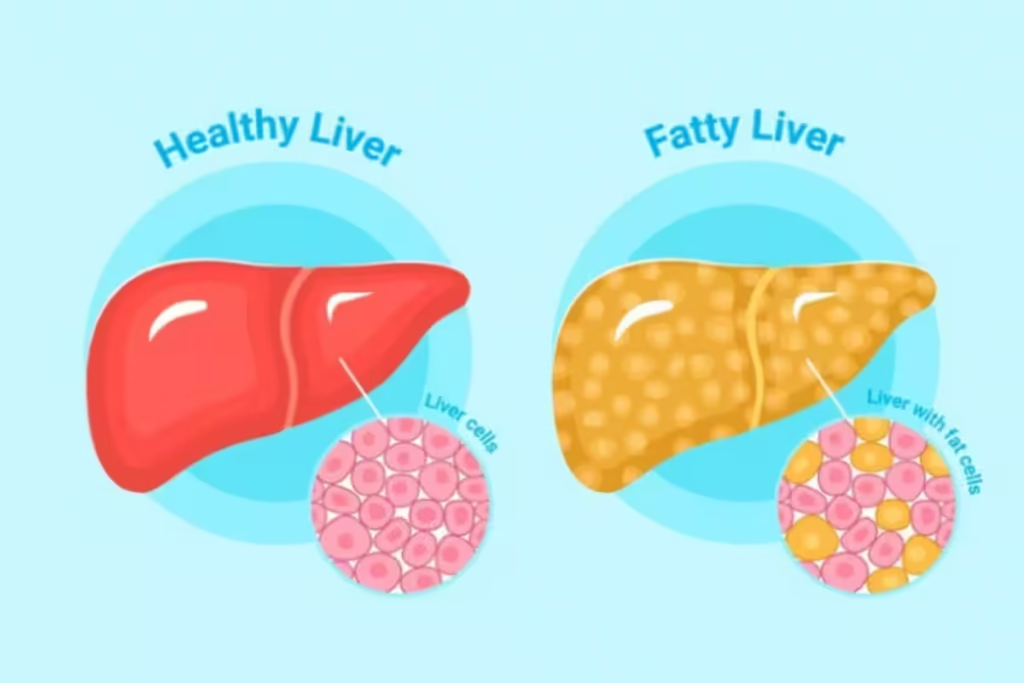
Fatty liver disease occurs when excess fat accumulates in the liver, leading to inflammation and potential damage. This condition can progress into more severe liver diseases such as cirrhosis or liver cancer. It often develops silently, with many people unaware they have it until more serious symptoms appear.
In this guide, we’ll explore the causes, symptoms, and types of fatty liver disease, and provide insights into its treatment. Whether you’re concerned about your own liver health or looking to understand this condition better, this article will offer helpful information on managing and preventing fatty liver disease.
Understanding Liver Disease

Liver disease includes a range of disorders that impact the liver’s ability to function effectively. These conditions can arise from infections, genetic factors, long-term alcohol abuse, autoimmune disorders, or metabolic issues. One of the most common liver conditions is fatty liver disease, which occurs when excess fat accumulates in the liver. If left untreated, fatty liver disease can progress to more severe liver damage, including cirrhosis or liver failure. Understanding the causes and symptoms of liver disease is crucial for prevention and treatment.
Common Types of Liver Disease
Hepatitis (A, B, C, D, E) – A group of viral infections that cause inflammation in the liver. These infections can lead to both acute and chronic liver conditions, potentially resulting in long-term damage if left untreated.
Fatty Liver Disease (NAFLD and AFLD) – A condition where fat accumulates in liver cells, disrupting normal liver function. Non-alcoholic fatty liver disease (NAFLD) is related to metabolic issues, while alcoholic fatty liver disease (AFLD) is caused by excessive alcohol consumption.
Cirrhosis – A severe condition characterized by the progressive scarring of liver tissue. It results from long-term liver damage, often due to chronic conditions like alcohol abuse or hepatitis, and can lead to liver failure.
Liver Cancer – A type of cancer that often develops as a result of chronic liver disease, including cirrhosis or hepatitis. The risk increases significantly with prolonged liver damage.
Hemochromatosis and Wilson’s Disease – Genetic disorders that cause an abnormal buildup of metals (iron in hemochromatosis and copper in Wilson’s disease) in the liver, leading to liver damage and other complications.
Liver Disease Symptoms
One of the main challenges in diagnosing liver disease early is that many symptoms are subtle and can resemble those of other illnesses. Often, the liver can continue to function even when it’s damaged, delaying the appearance of noticeable symptoms.
In the case of fatty liver disease, this can lead to a delay in diagnosis, as many individuals may not experience significant symptoms until the condition has advanced. Early detection is crucial for effective treatment, as untreated fatty liver disease can progress to more severe liver conditions, such as cirrhosis or liver failure.
Common Symptoms of Liver Disease
Fatigue and Weakness
Chronic tiredness is often one of the earliest signs of liver trouble, including fatty liver disease. The liver’s reduced ability to function properly can leave individuals feeling constantly weak and low on energy.
Jaundice
Jaundice, which causes a yellowing of the skin and eyes, occurs due to a buildup of bilirubin in the blood. This can be a clear indicator of liver dysfunction, such as in fatty liver disease, which impairs the liver’s ability to process waste products.
Abdominal Pain and Swelling
Discomfort or swelling in the upper right side of the abdomen may indicate inflammation or enlargement of the liver, a common sign of fatty liver disease or more advanced liver conditions.
Dark Urine and Pale Stool
Changes in the color of urine or stool can signal liver dysfunction. Dark urine can result from excess bilirubin in the bloodstream, while pale stools may indicate a problem with bile production.
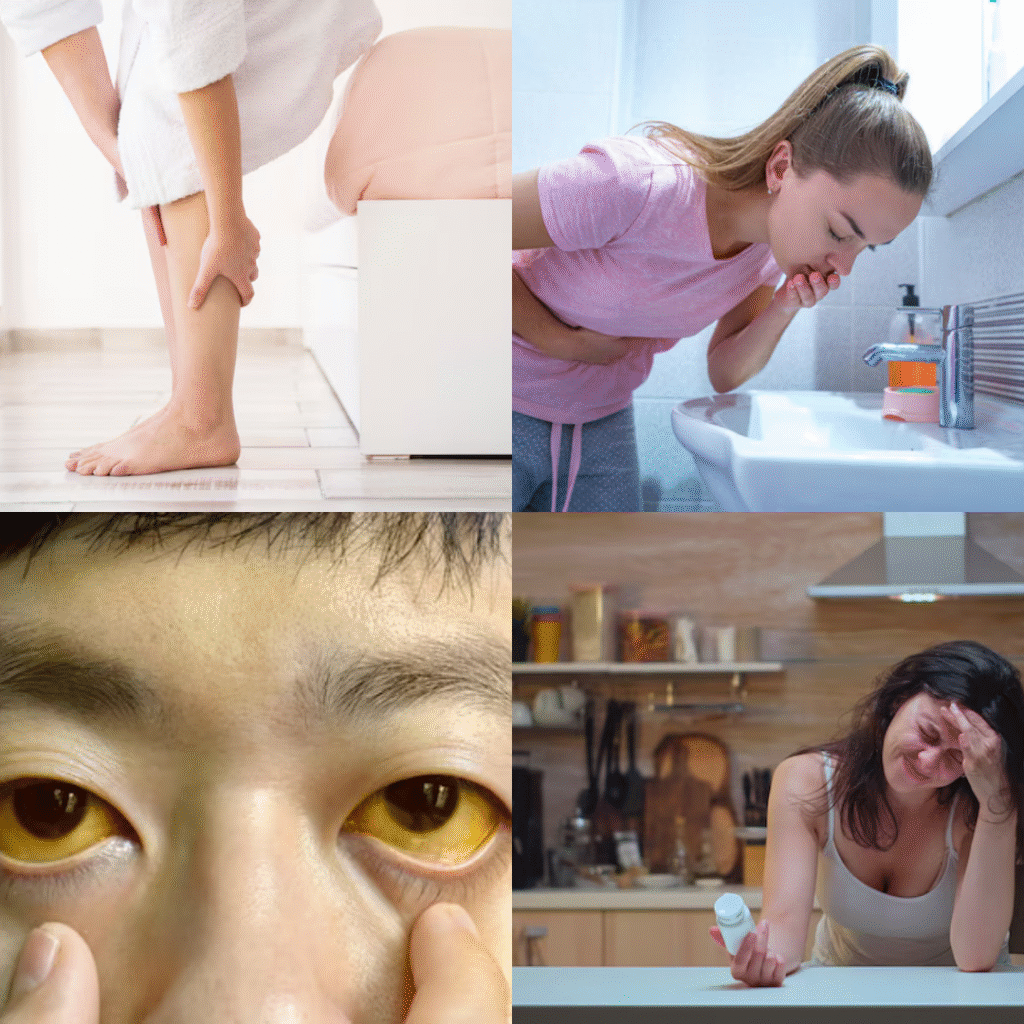
Nausea or Vomiting
Digestive symptoms like nausea or vomiting are often seen in individuals with fatty liver disease as the liver becomes less able to process food and toxins.
Loss of Appetite and Weight Loss
A poor-functioning liver can disrupt normal digestion, leading to a loss of appetite and unintentional weight loss, which are often seen in those with advanced liver issues like fatty liver disease.
Itchy Skin
Bile products can build up under the skin when the liver isn’t functioning well, causing itching. This symptom is common in people with liver diseases like fatty liver disease.
Swelling in Legs and Ankles
Reduced albumin production in the liver can lead to fluid retention, causing swelling in the legs and ankles, a sign of liver dysfunction.
Easy Bruising or Bleeding
The liver produces important clotting factors. When liver function is impaired by conditions such as fatty liver disease, the risk of easy bruising or bleeding increases.
Mental Confusion or Forgetfulness
Known as hepatic encephalopathy, this condition arises from the buildup of toxins in the bloodstream due to liver dysfunction, leading to mental confusion, forgetfulness, and other cognitive issues. This is often seen in more advanced stages of fatty liver disease.
What is Fatty Liver Disease ?
Fatty liver disease is a condition where excess fat accumulates in the liver cells. It is becoming more common, particularly in industrialized nations, as a result of factors like poor diet, obesity, and sedentary lifestyles.
In the early stages, fatty liver disease often does not present noticeable symptoms, making it difficult to diagnose. However, if left untreated, it can progress to more serious liver conditions like cirrhosis or liver failure. Early detection and lifestyle changes, such as improving diet and increasing physical activity, are key to managing the condition and preventing further liver damage.
Types of Fatty Liver Disease
Non-Alcoholic Fatty Liver Disease (NAFLD)
Occurs in people who drink little to no alcohol
Fatty liver disease can occur in individuals who consume little to no alcohol. Unlike alcoholic fatty liver disease, this form is related to factors such as poor diet, sedentary lifestyle, and other health conditions rather than alcohol consumption. It is commonly referred to as non-alcoholic fatty liver disease (NAFLD).
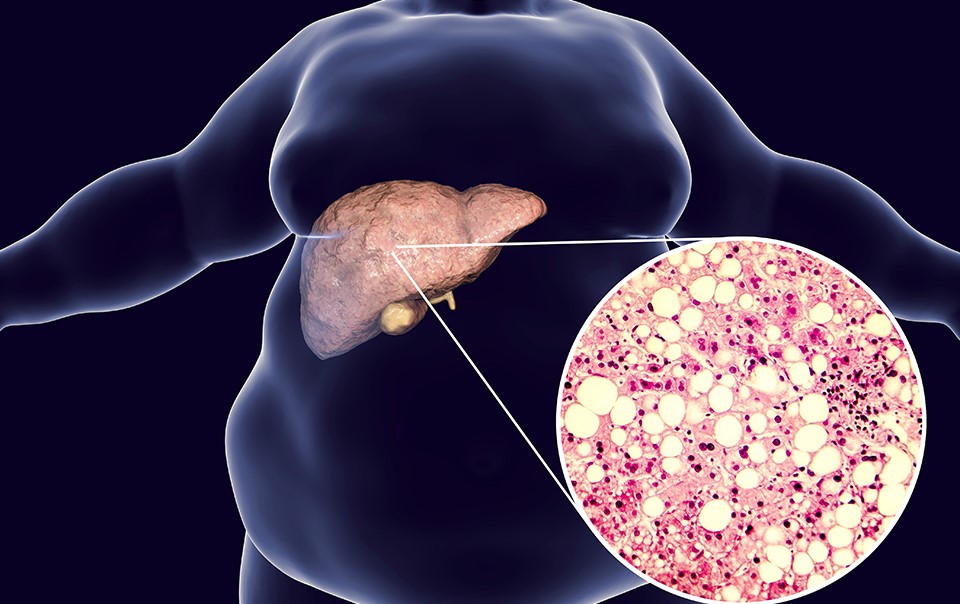
Closely linked to obesity, insulin resistance, type 2 diabetes, and metabolic syndrome
Fatty liver disease is often associated with obesity, insulin resistance, and type 2 diabetes. These conditions are part of the broader spectrum of metabolic syndrome, a cluster of risk factors that increase the likelihood of developing heart disease, stroke, and diabetes. The presence of these conditions significantly raises the risk of developing fatty liver disease.
Alcoholic Fatty Liver Disease (AFLD):
Directly related to heavy alcohol consumption
Alcoholic fatty liver disease develops as a result of excessive and prolonged alcohol intake. When the liver processes large amounts of alcohol, it can cause fat to build up in liver cells. Over time, this can impair liver function and lead to more severe liver conditions if not addressed.
Often reversible if caught early and drinking is stopped
If alcoholic fatty liver disease is detected in its early stages, it is often reversible. Stopping alcohol consumption allows the liver to begin healing, reducing fat accumulation and preventing further damage. Early intervention through lifestyle changes and medical guidance plays a crucial role in recovery.
Stages of Fatty Liver Disease
Simple Fatty Liver (Steatosis):
Fat accumulation without inflammation.
Usually harmless and reversible with lifestyle changes.
Non-Alcoholic Steatohepatitis (NASH):
Inflammation and liver cell damage, along with fat accumulation.
Can lead to fibrosis, cirrhosis, and liver cancer if untreated.
Fibrosis and Cirrhosis:
Progressive scarring of the liver that affects its function.
Cirrhosis is a late-stage, irreversible condition and may require liver transplant.
Causes and Risk Factors of Fatty Liver Disease
Obesity
High cholesterol and triglyceride levels
Insulin resistance and type 2 diabetes
Poor diet (high sugar and processed foods)
Sedentary lifestyle
Genetic predisposition
Rapid weight loss
Certain medications (e.g., corticosteroids, methotrexate)
Diagnosis of Liver Disease and Fatty Liver
Doctors diagnose liver disease using several methods. They usually begin with a physical examination to check for signs like swelling or tenderness. Blood tests are done to measure liver enzymes and assess overall liver function. Imaging studies such as ultrasounds, CT scans, or MRIs help visualize the liver’s condition and detect abnormalities. In some cases, a liver biopsy may be required to confirm the diagnosis and determine the extent of liver damage. These combined tools help provide an accurate diagnosis.
Diagnostic Tools
Liver Function Tests (LFTs): These blood tests check levels of liver enzymes such as ALT and AST, which help detect inflammation or damage in the liver.
Ultrasound: This imaging test is commonly used to spot fat deposits in the liver, making it helpful in diagnosing fatty liver disease.
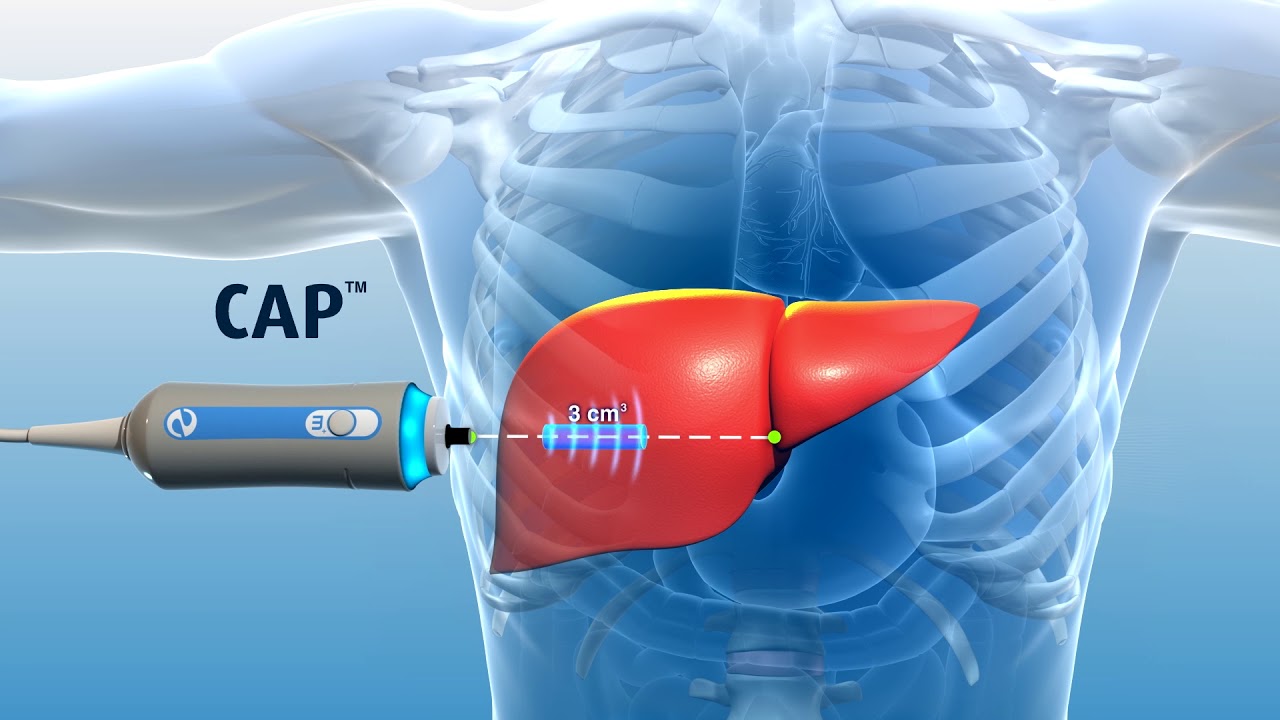
FibroScan: A non-invasive test that measures liver stiffness and fat content, helping assess the stage of liver disease.
CT Scan or MRI: These advanced imaging methods provide clearer, more detailed pictures of the liver to identify any abnormalities.
Liver Biopsy: In this procedure, a small tissue sample is taken from the liver to evaluate the degree of inflammation, fat buildup, or scarring (fibrosis).
Fatty Liver Treatment: A Holistic Approach
There is currently no FDA-approved medication specifically for NAFLD or NASH, making lifestyle changes the cornerstone of treatment. However, ongoing research offers hope for pharmacological options in the future.
Weight Loss
Losing 7–10% of body weight has been shown to reduce liver fat, inflammation, and fibrosis
Aim for a gradual weight loss (1–2 pounds per week) to avoid worsening the condition.
Dietary Changes
Avoid sugary drinks and processed foods.
Eat more fruits, vegetables, whole grains, and lean proteins.
Include omega-3 fatty acids (from fish or flaxseed).
Limit saturated fats and red meat.
The Mediterranean Diet is particularly beneficial for liver health.
Exercise
Regular physical activity improves liver enzymes and insulin sensitivity.
Aim for at least 150 minutes of moderate-intensity exercise per week (e.g., brisk walking, cycling).
Manage Blood Sugar and Cholesterol
Control diabetes and hyperlipidemia with medication, diet, and exercise.
Statins may be used safely under doctor supervision, even in liver disease.
Medication and Supplements
While no drugs are specifically approved for NAFLD/NASH, some may help:
Vitamin E (antioxidant): Can reduce liver inflammation in non-diabetic patients.
Pioglitazone: Used in diabetic patients; improves liver histology in some.
GLP-1 Receptor Agonists: New diabetes medications that promote weight loss and show liver benefits.
Advanced Treatments for Severe Fatty Liver Disease
Liver Transplant: For end-stage liver disease.
Experimental Therapies: Ongoing clinical trials for drugs targeting NASH fibrosis.
Bariatric Surgery: May be considered in severely obese individuals with advanced NAFLD.
Preventing Fatty Liver Disease and Maintaining Liver Health
Prevention is key, especially given that early-stage fatty liver is reversible. Here’s how to protect your liver long-term:
Maintain a Healthy Weight
Aim for gradual, steady weight loss through consistent habits rather than crash diets. Excess body fat, especially around the abdomen, increases the risk of developing fatty liver disease.
Eat a Balanced Diet
Choose whole, unprocessed foods like fruits, vegetables, whole grains, and lean proteins. A nutrient-rich diet supports liver function and helps manage fatty liver disease.
Be Physically Active
Including regular aerobic exercise and strength training into your weekly routine. Physical activity helps burn fat and reduce liver fat levels, improving outcomes for those with fatty liver disease.
Avoid Excessive Alcohol and Drug Use
Limit alcohol consumption and avoid recreational drug use. Both can worsen liver damage and contribute to the progression of fatty liver disease.
Get Regular Screenings
If you have conditions like type 2 diabetes, obesity, or high cholesterol, regular liver function tests can help detect fatty liver disease early and monitor its progression.
Get Vaccinated
Vaccines for hepatitis A and B can prevent infections that cause liver damage, especially important for individuals already managing fatty liver disease or other liver conditions.
Conclusion
Fatty liver disease is becoming a major health issue across the globe, affecting people of all ages and backgrounds. This condition often develops quietly, with few or no symptoms in the early stages. However, when identified early, fatty liver disease is usually preventable and even reversible. The key lies in raising awareness, recognizing the warning signs, and taking steps toward early diagnosis and care.
Timely medical attention and lifestyle changes are essential in managing fatty liver disease. These changes include improving your diet, staying physically active, and maintaining a healthy weight. Such actions can significantly reduce liver fat, improve overall liver function, and stop the condition from progressing to more serious stages.
Although researchers are still working to develop specific treatments for NAFLD (non-alcoholic fatty liver disease) and NASH (non-alcoholic steatohepatitis), we already have effective tools at our disposal. Healthy habits and regular medical checkups remain the most reliable ways to protect yourself from fatty liver disease.
FAQs
- What is fatty liver disease, and how serious is it ?
Fatty liver disease happens when too much fat builds up in the liver. In the early stages, it may not cause symptoms, but over time, it can lead to liver inflammation, scarring (fibrosis), cirrhosis, or even liver failure if not treated. - What causes fatty liver disease ?
Fatty liver disease can be caused by obesity, poor diet, lack of exercise, type 2 diabetes, high cholesterol, or excessive alcohol use. Some people may also be at higher risk due to genetics or certain medications. - Can fatty liver disease be reversed ?
Yes, in many cases, especially in the early stages, fatty liver disease can be reversed with healthy lifestyle changes. Losing weight, eating a balanced diet, exercising regularly, and avoiding alcohol can greatly improve liver health. - What are the symptoms of fatty liver disease ?
Fatty liver disease often has no symptoms in the beginning. As it progresses, it may cause fatigue, abdominal discomfort, weight loss, yellowing of the skin (jaundice), swelling, or confusion in severe cases. - How is fatty liver disease diagnosed ?
Doctors use blood tests to check liver enzymes, along with imaging tests like ultrasound or FibroScan to see fat buildup. Sometimes, a liver biopsy is needed to confirm the diagnosis and assess liver damage.

