Prostate health is a vital aspect of overall well-being for men, especially as they age. The prostate is a small gland located just below the bladder, responsible for producing seminal fluid that supports sperm health and mobility. Though small in size, it plays a major role in the male reproductive system.
As men get older, the prostate is more likely to develop issues such as inflammation, enlargement, or even cancer. Conditions like prostatitis, benign prostatic hyperplasia (BPH), and prostate cancer are common and can significantly impact quality of life. Early signs may include frequent urination, weak urine flow, or discomfort in the pelvic area.
Maintaining good prostate health involves a proactive approach that includes regular medical checkups, a nutritious diet, physical activity, and avoiding harmful habits like smoking. By staying informed and adopting healthy routines, men can reduce their risk of prostate-related issues and support their long-term health.

1. Understanding the Prostate
The prostate is a small, walnut-sized gland located below the bladder in men, playing a crucial role in the male reproductive system by producing fluid that nourishes and transports sperm. Despite its importance, it is often overlooked in general health discussions, making awareness and education essential.
As men age, the risk of prostate issues such as prostatitis, benign prostatic hyperplasia (BPH), and prostate cancer increases. Common symptoms of prostate problems include frequent urination, difficulty starting or stopping urination, and pelvic discomfort. Recognizing these signs early can lead to timely diagnosis and better management.
Focusing on prostate health through regular checkups, a balanced diet, exercise, and healthy lifestyle habits can significantly reduce the risk of complications. There are also effective treatments available, ranging from medication to minimally invasive procedures and surgery. Prioritizing prostate health helps support overall well-being and ensures a higher quality of life as men grow older.
Functions of the Prostate
Seminal Fluid Production: The prostate gland is responsible for producing approximately 30% of the fluid found in semen. This fluid contains essential enzymes, proteins, and minerals that help nourish and support sperm. Maintaining good prostate health ensures this important function continues efficiently.
Sperm Activation and Protection: The prostate contributes vital substances that protect sperm and improve their mobility. These fluids help sperm survive in the female reproductive tract, increasing the chances of successful fertilization. Supporting prostate health is key to preserving male fertility and reproductive performance.
Urinary Control: Because the prostate surrounds part of the urethra, it plays a significant role in regulating urine flow. A healthy prostate helps ensure proper urinary control, while any enlargement or inflammation can lead to discomfort or difficulty in urination. Focusing on prostate health can help prevent such urinary issues as men age.
2. Common Prostate Conditions
As men age, the risk of developing prostate-related issues increases. Some of the most common conditions include:
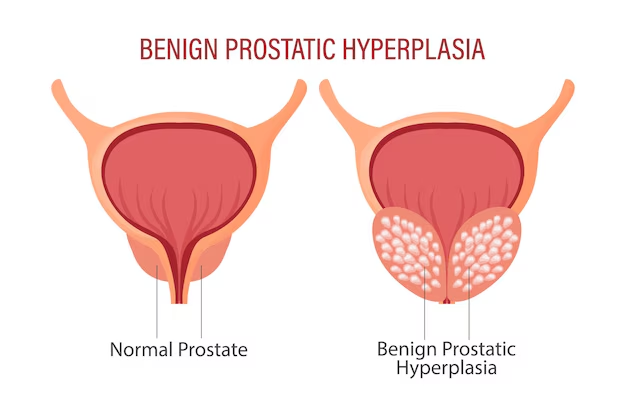
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland that commonly affects men over the age of 50. As the prostate grows, it can press against the urethra and interfere with normal urine flow, leading to symptoms such as frequent urination, difficulty starting or stopping urination, and a weak urine stream. While BPH is not cancerous, it can significantly impact quality of life if left untreated. Monitoring and managing BPH is an important part of maintaining prostate health. With proper care, lifestyle changes, and medical support, men can reduce discomfort and maintain good prostate health over time.
Symptoms:
Frequent urination, especially at night
Difficulty starting urination
Weak urine stream
Inability to completely empty the bladder
Causes:
Age-related hormonal changes
Genetic factors
Treatment:
Medications (alpha-blockers, 5-alpha reductase inhibitors)
Lifestyle changes
Surgery (e.g., TURP)
Prostatitis
Prostatitis is a condition characterized by inflammation of the prostate gland and can be either bacterial or non-bacterial in origin. It can affect men of all ages but is more common in younger and middle-aged men. Symptoms may include pelvic pain, painful urination, frequent urge to urinate, and discomfort during ejaculation. Bacterial prostatitis is usually caused by a urinary tract infection, while non-bacterial prostatitis may result from stress or other underlying health issues. Prompt diagnosis and treatment are important for relieving symptoms and preventing complications. Taking care of prostate health can help reduce the risk and severity of prostatitis.
Types:
Acute bacterial prostatitis
Chronic bacterial prostatitis
Chronic pelvic pain syndrome (CPPS)
Asymptomatic inflammatory prostatitis
Symptoms:
Pain in the groin, lower back, or genitals
Painful urination or ejaculation
Flu-like symptoms (in bacterial cases)
Treatment:
Antibiotics (for bacterial prostatitis)
Anti-inflammatory medications
Physical therapy
Prostate Cancer
Prostate cancer is one of the most common types of cancer affecting men, especially those over the age of 50. It usually develops slowly, and in many cases, it may not show noticeable symptoms in the early stages. As it progresses, signs such as trouble urinating, blood in urine or semen, and pelvic discomfort may appear. Early detection through regular screenings, such as PSA tests and digital rectal exams, is key to managing this condition effectively. Focusing on prostate health through regular checkups and a healthy lifestyle can help reduce the risk and support early diagnosis of prostate cancer.
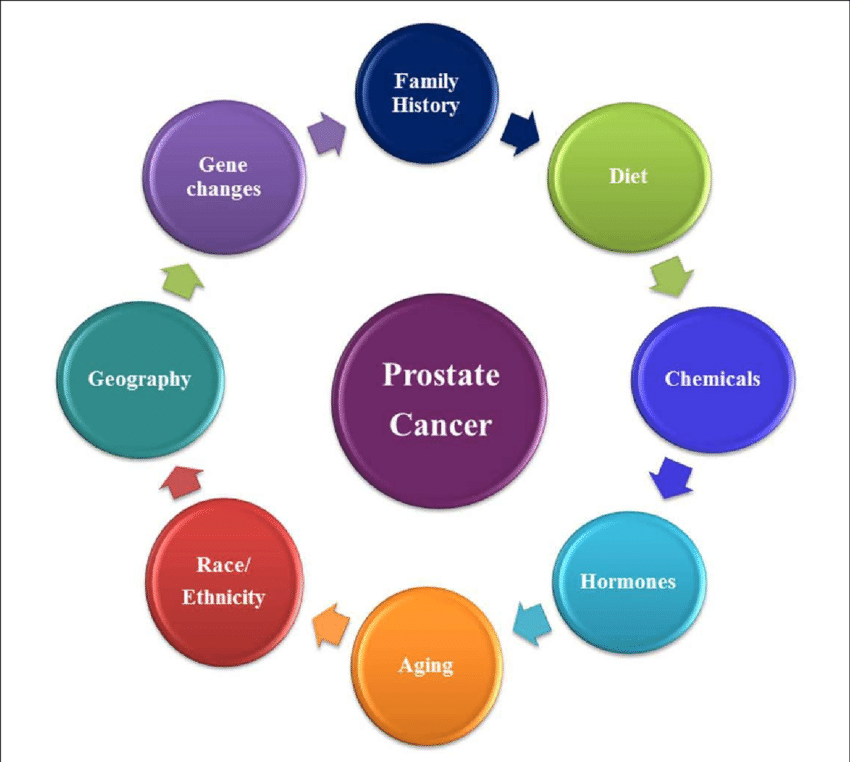
Risk Factors:
Age (risk increases after 50)
Family history
Race (higher incidence in African American men)
Diet and lifestyle
Symptoms
Trouble urinating
Blood in urine or semen
Erectile dysfunction
Bone pain (in advanced cases)
Diagnosis:
Digital rectal exam (DRE)
Prostate-specific antigen (PSA) blood test
Biopsy
Imaging (MRI, CT scans)
Treatment:
Active surveillance (for slow-growing cancers)
Surgery (prostatectomy)
Radiation therapy
Hormone therapy
Chemotherapy
Immunotherapy
3. Risk Factors Affecting Prostate Health
Understanding the risk factors associated with prostate issues is essential for prevention and early detection. Age is one of the biggest risk factors, with prostate problems becoming more common in men over 50. Family history, ethnicity, diet, and lifestyle choices also play a significant role in determining a man’s risk. African American men and those with close relatives who had prostate cancer are at higher risk. By recognizing these factors early and making informed health decisions, men can take proactive steps to support prostate health. Regular screenings and a healthy routine can significantly improve outcomes and reduce potential complications.
Age
The likelihood of developing prostate-related issues rises notably after the age of 50. As men grow older, natural hormonal changes and prostate enlargement become more common, increasing the risk of conditions such as BPH and prostate cancer. Regular monitoring is important to maintain prostate health during this stage of life.
Genetics and Family History
Men who have a close relative, such as a father or brother, with a history of prostate cancer or benign prostatic hyperplasia (BPH) face a higher risk of developing similar conditions. A family history suggests a genetic predisposition, making early screening and proactive prostate health management essential.
Diet and Lifestyle
Consuming a diet high in saturated fats, particularly from red meats and full-fat dairy products, has been linked to an increased risk of prostate problems. Additionally, a low intake of fruits and vegetables may deprive the body of essential nutrients that support prostate health. Lack of physical activity and obesity are also associated with a greater likelihood of developing BPH and prostate cancer. Adopting a balanced diet and active lifestyle can help lower these risks.
Hormonal Imbalance
Testosterone and its derivative, dihydrotestosterone (DHT), influence prostate growth and can contribute to BPH or cancer.
4. Maintaining Prostate Health
Diet and Nutrition
A healthy diet plays a vital role in supporting prostate function and maintaining overall prostate health. Eating a variety of nutrient-rich foods, including fruits, vegetables, whole grains, and healthy fats, provides the body with antioxidants and anti-inflammatory compounds that help protect the prostate. Reducing the intake of red meat, processed foods, and high-fat dairy can also lower the risk of prostate-related issues. Incorporating foods like tomatoes, leafy greens, nuts, and fatty fish may further promote prostate health and reduce the chances of developing conditions such as BPH or prostate cancer.
Foods That Promote Prostate Health:

Tomatoes: Rich in lycopene, an antioxidant linked to reduced prostate cancer risk.
Cruciferous Vegetables: Broccoli, cauliflower, and kale contain compounds that protect against cancer.
Fatty Fish: Omega-3 fatty acids in salmon and sardines reduce inflammation.
Green Tea: Contains antioxidants known as catechins.
Nuts and Seeds: Rich in zinc and selenium.
Foods to Avoid:
Red and processed meats
High-fat dairy
Excessive alcohol and caffeine
Regular Exercise
Regular physical activity is essential for maintaining prostate health. Exercise helps regulate hormone levels, supports a stronger immune system, and reduces the risk of obesity—factors that are closely linked to prostate conditions. Staying active can lower the chances of developing issues like benign prostatic hyperplasia (BPH) and prostate cancer. Activities such as walking, swimming, or strength training not only improve overall fitness but also contribute to long-term prostate health. Making exercise a part of your daily routine is a powerful way to support both general wellness and prostate function.
Regular Checkups
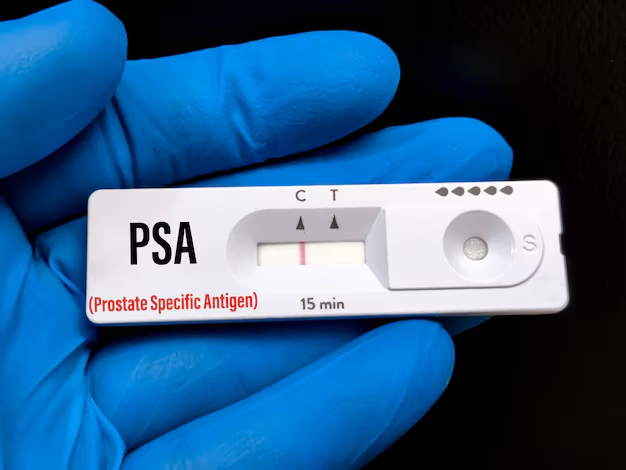
Routine screenings are a key part of maintaining prostate health, as they help detect potential problems early, often before symptoms appear. Tests like the PSA blood test and digital rectal exam allow for timely diagnosis and treatment, greatly improving outcomes and reducing the risk of serious prostate conditions.
Annual PSA tests and DREs for men over 50 (or earlier if at higher risk)
Monitoring urinary function and overall reproductive health
Stress Management
Chronic stress can have a negative impact on hormone levels and immune function, both of which are crucial for maintaining prostate health. Prolonged stress may increase the risk of prostate issues by disrupting the body’s natural balance. To manage stress effectively, techniques such as yoga, meditation, and deep breathing exercises can be highly beneficial. These practices not only help reduce stress but also promote relaxation and improve overall well-being. By incorporating stress-reduction techniques into your daily routine, you can support both mental health and prostate health in the long term.
5. Supplements and Natural Remedies
Saw Palmetto
Saw palmetto is commonly used to alleviate symptoms of benign prostatic hyperplasia (BPH). It is believed to work by inhibiting the action of dihydrotestosterone (DHT), a hormone that can contribute to prostate enlargement. By reducing DHT levels, saw palmetto may help improve urinary function and decrease the discomfort associated with BPH.
Beta-Sitosterol
Beta-sitosterol is a plant-derived compound known for its potential to improve urinary symptoms related to BPH. It works by supporting healthy urinary flow and reducing inflammation in the prostate. Regular use of beta-sitosterol has shown promise in improving overall prostate health and easing symptoms such as frequent urination.
Pygeum
Pygeum is an herbal extract from the African plum tree, traditionally used to address prostate-related issues. It is particularly beneficial for improving urinary symptoms associated with BPH, such as frequent or painful urination. Pygeum also helps reduce inflammation within the prostate, promoting better urinary function and overall prostate health.
Zinc and Selenium
Zinc and selenium are essential minerals that play a crucial role in maintaining prostate health. Zinc is involved in regulating prostate function, while selenium acts as an antioxidant, protecting prostate cells from damage. Together, these minerals support immune function, reduce inflammation, and contribute to the prevention of prostate-related issues.
6. Screening and Early Detection
Early detection significantly improves treatment outcomes, particularly for prostate cancer.
Prostate-Specific Antigen (PSA) Test
The Prostate-Specific Antigen (PSA) test is a blood test that measures the level of PSA, a protein produced by the prostate gland. Elevated PSA levels can indicate various prostate health issues, such as inflammation, enlargement (BPH), or even prostate cancer. Regular PSA screenings are an important part of monitoring prostate health, especially in men over 50 or those with a family history of prostate conditions. Early detection through PSA testing can help identify problems before symptoms arise, allowing for timely intervention.
Digital Rectal Exam (DRE)
A Digital Rectal Exam (DRE) is a physical examination where a doctor checks the prostate for abnormalities by inserting a gloved finger into the rectum. This test allows the doctor to feel the size, shape, and texture of the prostate and detect any lumps, hard areas, or irregularities that may indicate potential prostate health issues, including cancer. The DRE is a standard part of prostate health checkups and is often used in conjunction with the PSA test for a more thorough assessment.
Imaging and Biopsy
Imaging techniques such as MRI and ultrasound may be used to identify suspicious areas of the prostate that may require further investigation. These non-invasive tests help doctors visualize the prostate and detect abnormalities, such as tumors or enlarged areas. If imaging results are concerning, a biopsy may be recommended to collect tissue samples from the prostate for analysis. A biopsy provides a definitive diagnosis, helping doctors determine whether prostate cancer or other conditions are present, allowing for appropriate treatment and management of prostate health.
7. Prostate Health Myths and Facts
Myth: Prostate problems only affect older men.
Fact: While it is true that age increases the risk of prostate health issues, such as benign prostatic hyperplasia (BPH) and prostate cancer, prostatitis can affect men of all ages. Prostatitis, an inflammation of the prostate, is commonly seen in younger and middle-aged men, often caused by bacterial infections or other factors unrelated to aging. It’s important to monitor prostate health at all stages of life to detect and address any issues early, regardless of age.
Myth: High PSA always means cancer.
Fact: While an elevated Prostate-Specific Antigen (PSA) level is often associated with prostate cancer, it does not always indicate cancer. PSA levels can also rise due to other prostate health conditions such as BPH (benign prostatic hyperplasia), prostatitis, or even recent ejaculation. An elevated PSA level warrants further testing and investigation to determine the underlying cause, and it’s crucial not to jump to conclusions without a complete evaluation by a healthcare professional.
Myth: A prostate exam is painful.
Fact: A Digital Rectal Exam (DRE), which is commonly performed to check prostate health, may cause some discomfort, but it is usually quick and rarely painful. During the exam, a doctor gently inserts a gloved finger into the rectum to assess the size, shape, and consistency of the prostate. While it may feel awkward or uncomfortable, the procedure is essential for detecting abnormalities, and the benefits of regular prostate exams far outweigh any temporary discomfort.
8. Living with Prostate Conditions
Living with prostate-related issues can be challenging, but management strategies and support are available.
Emotional Impact
Dealing with prostate cancer or chronic prostatitis can significantly affect emotional well-being, leading to anxiety or depression. It’s important to address the emotional side of prostate health, and seeking counseling or joining support groups can provide valuable assistance. Support systems help improve mental health and coping strategies.
Sexual Health
Many prostate conditions and their treatments affect sexual function. Options include:
Medications (e.g., PDE5 inhibitors like Viagra)
Pelvic floor therapy
Couples counseling
Incontinence and Urinary Control
Bladder training and Kegel exercises are effective techniques to improve urinary symptoms, especially after prostate surgery or in cases of BPH. These exercises help strengthen pelvic muscles, enhance bladder control, and reduce leakage, supporting overall prostate health and recovery. Regular practice can improve quality of life and urinary function.
9. Emerging Research and Future Directions
Precision Medicine: Precision medicine involves the use of genetic profiling to create personalized treatment plans for individuals with prostate health issues, including prostate cancer. By analyzing a patient’s genetic makeup, doctors can better understand how the cancer is likely to behave and respond to various treatments. This approach allows for more targeted therapies, minimizing side effects and increasing the effectiveness of treatment.
Immunotherapy: Immunotherapy is showing promising results in the treatment of advanced prostate cancer, particularly in cases where traditional therapies may not be as effective. This treatment works by stimulating the body’s immune system to recognize and attack cancer cells more efficiently. Ongoing research continues to explore the potential of immunotherapy in improving outcomes for patients with advanced or metastatic prostate cancer.
Liquid Biopsies: Liquid biopsies are an innovative, non-invasive method for detecting cancer at early stages, including prostate cancer. This technique involves analyzing blood samples to identify cancer-related genetic material or other biomarkers. Liquid biopsies provide a less invasive alternative to traditional biopsies and are being increasingly used for early detection, monitoring treatment progress, and assessing recurrence, all while reducing patient discomfort.
New Imaging Techniques: Advances in imaging technologies are enhancing the accuracy of prostate cancer diagnosis and monitoring. Techniques such as multiparametric MRI and PET scans offer clearer, more detailed images of the prostate, allowing doctors to detect abnormalities, stage the cancer more precisely, and monitor treatment responses. These new imaging methods improve the ability to identify small tumors, monitor disease progression, and personalize treatment plans, ultimately leading to better patient outcomes.
Conclusion

Prostate health is a crucial aspect of overall well-being for men, particularly as they age. The prostate plays a key role in reproductive function, and maintaining its health is essential for quality of life. As men get older, the risk of developing prostate conditions such as benign prostatic hyperplasia (BPH) and prostate cancer increases, making awareness and care even more important.
Recognizing the symptoms of prostate issues, such as frequent urination, difficulty starting or stopping urination, or pain in the pelvic area, is vital for early detection. Adopting a healthy lifestyle, including regular physical activity, a balanced diet, and stress management, can also support prostate health and reduce the risk of complications.
Regular medical checkups and screenings are essential to monitor prostate health. With ongoing advancements in medical research and treatment options, the outlook for men with prostate conditions continues to improve, offering better prevention, early detection, and treatment possibilities for a healthier future.
FAQs
- What are common symptoms of prostate issues ?
Common symptoms of prostate issues include frequent urination, especially at night, difficulty starting or stopping urination, a weak or interrupted urine stream, pain or discomfort in the pelvic area, and blood in the urine or semen. If you experience any of these symptoms, it’s important to consult a healthcare professional. - At what age should men start monitoring their prostate health ?
Men should begin monitoring their prostate health around the age of 50, or earlier if they have a family history of prostate cancer or other risk factors. Regular screenings, such as PSA tests and digital rectal exams (DRE), can help detect potential issues early. - How can I maintain good prostate health ?
Maintaining good prostate health involves adopting a healthy lifestyle, including a balanced diet rich in fruits and vegetables, regular exercise, managing stress, and avoiding smoking and excessive alcohol. Regular checkups and screenings are also important for early detection of any potential issues. - Is an elevated PSA level always a sign of prostate cancer ?
No, an elevated PSA level doesn’t always indicate prostate cancer. PSA levels can be elevated due to other conditions such as benign prostatic hyperplasia (BPH) or prostatitis. Further testing, such as a biopsy, may be needed to determine the cause of the elevated PSA. - What treatments are available for prostate cancer ?
Treatment options for prostate cancer vary depending on the stage and aggressiveness of the cancer. Common treatments include surgery, radiation therapy, hormone therapy, chemotherapy, and immunotherapy. In some cases, active surveillance may be recommended for slower-growing cancers. Discussing treatment options with a healthcare provider is essential to determine the best approach for each individual.

